In traditional healthcare, routine care is often ignored or delayed due to out-of-pocket costs, inconvenience, or conditioning that suggests healthcare is best saved for somewhere in the future (or an emergency). It’s a relatable snapshot of a hectic world that can move too quickly for its own good.
Similarly, the notion that the healthcare system is best saved for catastrophic issues is not only costly to organizations — it’s also harmful to members’ long-term health.
The truth is this: Healthcare is about caring for real people in a holistic way — and there’s no better place to do that than in primary care.
Primary care as a foundation
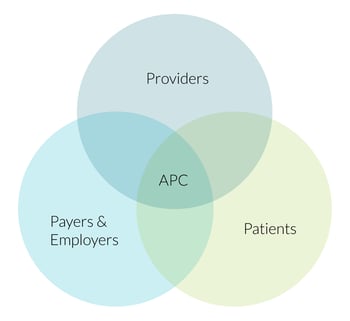 Unlike the traditional healthcare models built to generate reimbursement claims in exchange for services provided, advanced primary care (APC) is an evolution of primary care that aligns organizations, providers, and patients around improving health outcomes for patients.
Unlike the traditional healthcare models built to generate reimbursement claims in exchange for services provided, advanced primary care (APC) is an evolution of primary care that aligns organizations, providers, and patients around improving health outcomes for patients.
APC delivers 80-90 percent of all necessary care. Care centers act as the medical hub for members — a convenient place where patients visit with providers for routine or preventive matters or connect with a health coach to collaborate on positive behavior changes.
By strengthening the patient-provider relationship, unseen (or unknown) health circumstances can be greatly reduced or removed over time. Consider these common scenarios:
-
A man in his mid-30s tends to avoid routine or preventive care because it doesn’t occur to him.
The man generally describes himself as healthy although he feels run down and tired much of the time. A newer member of an APC network, he decides to schedule a preventive exam where the provider suggests additional blood tests for a sinus infection and allergies. He meets a health coach as part of the appointment and shares about frequent work-related stress and how he smokes to alleviate some of the pressure in his work life. At a convenient follow-up appointment, the man learns he has been living with sinusitis and is allergic to tobacco. He receives a treatment plan for sinusitis and works with a health coach to quit smoking. The man reports feeling more vitality due to the absence of sinusitis and the ways he’s replaced smoking (and the related sinus congestion) with healthier coping strategies.
-
A woman in her late 30s gets a cervical cancer screening at her primary care provider
and mentions she would like to take a more proactive role in getting healthier, but limited time often gets in her way. The APC provider introduces the woman to a health coach during the same annual checkup and begins a relationship. The woman learns to implement meditation, stretch breaks, and virtual yoga classes that improve her long-term health, happiness, and wellness —all while fitting into her busy life.
APC provides a robust set of routine and preventive services to address root causes that in turn reduce or remove symptoms or conditions before they manifest as chronic illnesses.
How apparently healthy populations are key to cost control

The phrase “out of sight, out of mind” may be helpful in certain contexts but it’s not a winning formula when it comes to lowering overall healthcare costs and improving members’ long-term health outcomes. The population segment known as “apparently healthy members” show no outward sign of health issues. They make up 75 percent of the population and account for 20 percent of health-related costs. But those statistics only last for so long.
When an apparently healthy member skips an annual physical or a routine appointment, they’re missing a valuable chance to achieve better health and to catch health issues that could significantly impact wellness and drive up the overall cost of care if left untreated. By failing to engage primary care services, members leave providers in the dark about the best way to provide personalized care.
APC offers the most simple, accessible, and affordable entry point for members to build relationships with providers. It’s an environment where the biopsychosocial needs of members can be addressed and nurtured — and apparently healthy members can improve behavior choices and get treatment for things that would later become significant cost burdens.
Primary care reduces the need for costly services

“By spending time with patients, primary care physicians have the opportunity to get a full picture of the patient’s health, including outside factors that influence it. In particular, providers in value-based care models, who are responsible for the total cost of care for their patients, have every incentive and more flexibility than most insurers to offer services and programs that lead to better care and lower costs.”
— Excerpt from Innovation in Medicare Advantage Begins With Doctors, American Journal of Managed Care
For Dr. Christopher Chen (the author of the article above), robust primary care models are at the center of successful healthcare plans. Chen notes a benefit plan that includes more time for physician-patient interaction, empathetic listening practices, and coordinated care results in better care and lower costs.
In fact, the article cites a 33.6 percent reduction in ER visits, 28 percent fewer hospital admissions, and 25.7 percent fewer inpatient hospital days on average, when utilizing coordinated care models similar to Vera Whole Health.
At Vera, these practices are at the core of our APC model. So what’s included?
Our approach to primary care
Since pioneering APC in 2012, the model has transformed healthcare by the way organizations pay, how patients engage, and how providers deliver care. Our APC model includes:
- Attentive providers who get to practice the full breadth of their training and experience to treat patients rather than simply act as a gatekeeper to specialty care.
- Longer appointments to ensure the holistic needs of patients are empathetically heard and attentively addressed.
- Clinically integrated health coaches that support patients to take a more proactive role in their lifestyle improvements and health goals.
- Integrated care coordination working as a behind-the-scenes advocate for patients by coordinating specialty care, including follow-up and integration into the member’s care plan.
- Behavioral health professionals to support patients’ behavioral and/or mental health concerns including anxiety, trauma, depression, addiction, ADHD, and more — issues that have only become clearer throughout the global pandemic.
- Preventive services like our Annual Whole Health Evaluation that includes a 60-minute provider wellness exam, biometric screening, member health assessment, and an introduction to a health coach.
- Low- or no-cost primary care services for members including routine and preventive care.
When patients utilize APC centers and take advantage of preventive care services, significant improvements follow — and patients are empowered to change their behavior and live healthier lives.
And the vast majority of it is happening in APC centers.
Learn more about how advanced primary care can protect your bottom line and improve health outcomes at the same time.
This post is an update of an article we first published on February 15, 2018.