APC Defined
The Vera APC model is the next evolution of primary care, delivering the essential 1:1 patient-provider relationship through informatics, referral management and care coordination, integrated health coaching, and more.
A Proven Value-Based Model That Drives Real Outcomes
Download as PDF 30 Min Read
It was developed by Vera Whole Health in 2012, and when implemented across Vera’s care delivery network in 2019, APC demonstrated that improved outcomes and reduced total cost of care were both possible.
Now, Vera and Castlight Health have combined to pioneer and scale value-based care in the commercial market.
Join us as we explore what APC is and the difference it makes when done right.
Traditional fee-for-service healthcare models are broken, but there is another way — one with proven results. APC, delivered with a proven partner, helps you put an end to skyrocketing healthcare costs while driving significant improvements in members’ engagement and health outcomes.
The Vera APC model is the next evolution of primary care, delivering the essential 1:1 patient-provider relationship through informatics, referral management and care coordination, integrated health coaching, and more.
APC is only possible if providers, payers, and employers agree to align incentives around health outcomes rather than around a volume-based, fee-for-service approach.
When APC is structured with incentives aligned to improve health, instead of driving volume, care teams practicing in this model can measurably improve the health of their patient population while dramatically reducing the total cost of care.
The following capabilities are required:

An informatics platform segments the population by risk, allowing the care team to target the highest risk, most impactable segments first. Adherence is boosted and members are encouraged to seek the care they need through customized outreach that speaks to their specific health situations. Smart analysis of claims data yields actionable insight, opens opportunities to increase appropriate utilization, and enables care teams to close care gaps.
Vera providers use high-value, low-cost specialty networks, allowing them to steer patients to the appropriate specialists when necessary. Care teams not only schedule and manage specialty appointments, they also, most importantly, schedule follow-ups when necessary and integrate specialty plans into members’ overall care plans.

Clinically integrated Vera whole health coaches are trained in the Transtheoretical Model (TTM) to help patients move through the five stages of change, improving their lifestyles and achieving life goals. Because behavior change cannot be prescribed, Vera health coaches are essential stakeholders on APC care teams.
APC makes it possible to deliver 1:1 population health. Even on a 1:1 basis, population health is rooted in a firm understanding of the segments that make up a population and a strategy for providing the most appropriate care to each.
Prevailing wisdom says it’s not possible to improve the health of the polychronic segment of a population and that providing these patients with the highest quality care at the most affordable cost is the best that can be achieved.
For example, some cases can include cancer, premature births, and Alzheimers, where the focus is on high quality care at a good value and not prevention. Any improved outcomes and/or reductions in costs need to come from the next two segments.
APC is well-designed to improve outcomes for the at-risk segment. Members in this segment live with underlying conditions that can benefit from proactive care and behavior change. APC enables care teams to take advantage of informatics to identify which at-risk members can most benefit from care, making sure they receive the most appropriate care first.
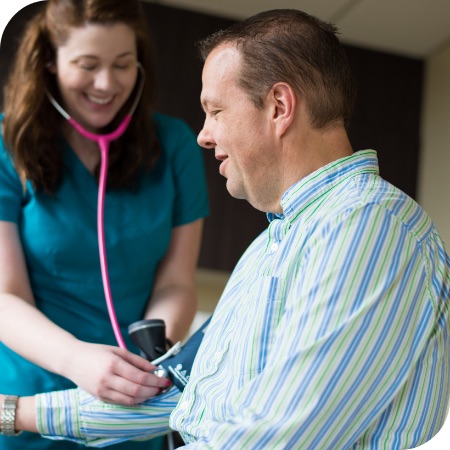
Once engaged, at-risk patients benefit from the incredible care experience afforded by the Vera APC model. True primary care, with its long, trust-building provider appointments, ensures these patients get the right type of treatment, health coaching, and behavior coaching to help them make the positive behavior changes that will improve their long-term health outcomes. Additionally, integrated care teams enable any required specialists to perform at their highest level due to the in-depth collaboration and communication provided by the member’s primary care team.
A different but no less effective effort is aimed at understanding and appropriately treating the third segment — people who appear healthy, but may have underlying health issues that are unseen because they don’t access care.
This segment of people, containing those who haven’t generated a healthcare claim, is a huge blind spot in fee-for-service primary care practices, because providers don’t have the insights afforded by informatics or the support from an integrated, personalized digital navigation platform. Supporting this segment starts with preventive care, including screenings for common diseases found among members of their particular population, and it continues with a more informed approach as this segment of the population engages.
When implemented with the right partner, APC delivers three key results that justify redistributing benefit funds to more primary care:
Health outcomes are improved over time by leveraging informatics and claims data to tailor care so that it addresses the care gaps and specific needs of a population. APC’s strong emphasis on preventive care, the increased access it provides to members, and its focus on behavior change mean that these outcomes can be sustained over time.
APC requires an upfront, increased financial allocation toward primary care. This investment drives more utilization through primary care, which in turn reduces utilization of uncontained downstream care across other portions of the healthcare system. The result is a dramatic return on investment through a reduction in total cost of care — fewer specialist care visits, decreased hospital and emergency department utilization, and even lowered drug costs.
There’s no more powerful experience for a patient than to know and trust their primary care team. The wraparound experience — where a patient feels heard, known, and empowered — meets them where they are, increasing satisfaction and engagement exponentially. In fact, members benefitting from Vera’s APC model consistently yields satisfaction scores above 4.6 out of 5.

Dr. Kevin Wang
Chief Medical Officer, Vera Whole Health
Advanced Primary CareAt Vera, we’re not only bringing in more advanced care practitioners (like MPs or NPs) and using a care team to coordinate care like many others are in the industry, but with APC we’re also adding behavioral change management, health coaching, and data analytics to drive it.
Our model isn’t about doing more with less. We’re about doing a lot more with the right team so that there are fewer gaps in care for the patient.
This stands in stark contrast to the typical focus on increasing productivity. For example, physicians who were able to serve a patient panel of 2,000 with one medical assistant were challenged to come up with ways to serve 4,000 without adding an additional provider. This wasn’t really possible without a significant drop in the quality of care. This is why our APC model is so revolutionary. Rather than focusing on productivity, it achieves increased quality and health outcomes at a lower cost by providing whole person care in an environment that emphasizes outcomes over efficiency.
True APC is here, and it’s a model where everyone wins: payers, employers, patients, and providers.
In the Vera value-based APC model, patients receive the care they need to be healthy (and not just the care needed for providers to meet fee-for-service quotas).
With Vera, patients benefit from three differentiators:
Providers move beyond symptom management because they have the time to explore the underlying issues beneath those symptoms, including physical issues and all the social determinants that affect health. Once these are uncovered over time, a plan can be developed to address them.
When APC is backed by an employer or provided by a payer as part of a health plan, care is then delivered at little to no cost to the patient. That’s a huge benefit, especially at a time when many patients ignore their health because they can’t afford treatment or defer care due to high co-pays or deductibles.
The APC model also helps patients experience the best of both worlds: the resources they need for a healthy lifestyle and healthcare that doesn’t bleed them dry.
This emphasis on individualized and efficient support has always existed in Vera care centers.
When APC is backed by an employer or provided by a payer as part of a health plan, care is delivered at little or no cost to the patient.
Self-insured employers get four key benefits from APC:
When self-insurers pair with APC, they gain more control over their benefits and plan design, reclaim consistency over a key part of their balance sheet, and retain lower overall costs of care. This helps employers avoid a cycle of increasing healthcare costs, forcing them to choose between reducing benefits or cost-shifting to their workforce to stay solvent.
APC’s proven results lead to healthier employees — and healthy employees are happier, more present, and more engaged in their workplaces. APC empowers and educates employees to take greater ownership of their health goals with the support of a primary care model focused on preventive health and improved well-being.
Employers who decide to implement APC with the help of a proven partner can dramatically enrich the healthcare benefits they provide, improving health outcomes while also flattening the curve of their benefit costs. This case study explains how.
Today’s workforce (the largest percentage of which is made up of Millennials) is looking for better healthcare options — options that are convenient, meaningful, and focused on their holistic health. APC allows employers to provide just that and, as a result, gain a competitive recruiting advantage. Learn more about how to meet the needs of Millennial employees here.
When self-insurers pair with APC, they gain more control over their benefit and plan design, reclaim consistency over a key part of their balance sheet, and retain lower overall costs of care.
Payers looking to build a competitive advantage in their markets will set themselves apart from their competition in five specific ways when they implement APC:
APC provides 80-90% of the care in the primary care context — essentially, it provides a one-stop shop for the healthcare needs of most members. With analytics, care coordination, virtual care, and health coaching integrated into the APC model, payers can improve outcomes across large populations and drive down total cost of care.
Payers can address the primary care shortage within their regions by embedding dedicated primary care access for members into health plans. With little to no cost to members and primary care teams who focus on these populations, payers remove access barriers (physical, financial, and even cultural) that would otherwise depress primary care utilization and frustrate their members. Integrated virtual care options provide an even greater level of convenience to members limited in their ability to access care.
For payers who serve Medicare Advantage members, APC enables improvement of HEDIS and star measures. In addition to CMS bonuses, payers also see financial returns from improved risk adjustment (RAF increases) and total cost of care reductions.
APC enables longer appointment times with an emphasis on empathetic listening. This allows members more time and space with their Vera care teams, allowing those teams to get at the root of their health issues. The result is that members feel heard — sometimes for the first time in their lives.
Payers signal value with APC and create the right alignment with their partners and across the system. Getting into care delivery with APC changes the conversation from renewals, authorizations, and networks to population health, well-being, and communities.
With analytics, care coordination, virtual care, and health coaching baked into the APC model, payers can improve outcomes across large populations and drive down total cost of care.
APC isn’t just a model that works for those who are receiving care or paying for it. It is also a model in which those who deliver care thrive. There are three main reasons for this dynamic:
In the APC model, financial incentives are based on the quality of care provided, not reimbursement for procedures. There’s no reason to rush through as many appointments as possible over the course of the day. As a result, providers spend more time with each patient.
Because APC focuses on providing 80-90% of care in the primary care setting, providers are encouraged to do more than simply serve as a gatekeeper to specialty care. They become the key medical provider to their patients, using the full scope of their training and skills to build relationships that drive improved outcomes for their patients.
In addition to having more time with patients and the incentive to provide whole health care to their patients, care teams also have the necessary support. At Vera, care teams are structured with health coaches and allied staff members supporting providers. Whole health coaches, who are experts in behavior change, and behavioral health professionals also offer additional support, helping patients with behavioral or mental health concerns.
In the APC model, financial incentives are based on the quality of care provided, not reimbursement for procedures. As a result, a provider typically sees half as many patients in a single day and spends more with each.
The most recent addition to the APC model arrives via our partnership with Castlight Health.
Vera & Castlight Health
Together, Vera and Castlight Health are transforming how patients engage with healthcare, how providers deliver care, and how payers and employers pay for healthcare. This partnership combines Castlight’s leading health navigation technology with Vera’s proven Advanced Primary Care model to provide a seamless member experience that drives results, and delivers large-scale innovation across the commercially-insured market.
Castlight’s data and technology enhances APC’s ability to reduce total cost of care, improve quality and outcomes, deliver best-in-class patient and member experience and address health equity for underserved populations.
Vera developed APC in 2012. Then we disrupted the industry by implementing it across our care network in 2019. In 2022, we’re revolutionizing healthcare even further by partnering with Castlight Health to expand our capabilities to help patients and providers navigate the complexities of healthcare.
Here are the four healthcare models and approaches that influenced and shaped what APC is today:

Managed care has been used as a framework for benefits plans for decades. It promises to centralize patient care within a single network or provider system, aimed at containing costs and improving patient health outcomes.
In concept, managed care makes sense. In practice, it didn’t work. It ended up simply controlling access to care in order to reduce costs, rather than also focusing on outcomes.
In a traditional managed care environment, patients are incentivized to use in-network providers and specialists, regardless of provider cost or quality. And, they’re punished financially for getting care outside their networks, whether it’s a wide PPO, or narrow HMO. But constraining patients to a network, no matter how large or small, doesn’t necessarily mean better health outcomes. Especially if the network is based on the reactive, sick-care system where symptom control and disease management are nothing more than Band-Aids on underlying health problems.
APC fulfills the original promise of managed care. Instead of simply forcing patients into a narrow network in order to control costs, APC puts its primary focus on outcomes. The best way to achieve outcomes is to place primary care at the center of the healthcare ecosystem and utilize it to provide the majority of care. At Vera, we provide 80-90% of care in the primary care context.
Inevitably, some patients do need to be referred to specialist care. When this happens, we refer patients to the highest value specialists (highest quality for the lowest cost) and then manage their follow-up at their Vera care center, where the help they need is integrated with their overall care plan.

ACOs were designed to hold groups of providers accountable, across different care settings, for the cost and quality of care provided to a defined group of specified members.
The whole point was to give providers an incentive to work together and better manage patient care. This is a good approach because it placed an emphasis on effective primary care and its role in coordinating and managing care to drive down unnecessary costs.
But there’s a significant dilemma with ACO: what about everyone else? And, beyond that, for patients who were part of an ACO (which might only have been a few on any given week), it was impossible for care teams to suddenly shift course midstream to provide higher quality care at a lower cost.
Most care teams wouldn’t know if a patient was part of an ACO to begin with. Even if they did, those teams didn’t have the time or resources to offer anything more for these patients than what they provided for everyone else.
APC builds on the concept of an ACO by aligning financial incentives around value — reimbursement based on outcomes (and total cost of care) rather than services, which means providing the highest quality care at the most affordable price. There is one fundamental difference. In the ACO model, providers and care teams only provided value-based care for those patients that were members of the ACO, while working on a traditional fee-for-service model for other patients. In the APC model, all patients are treated in a value-based arrangement that prioritizes the right health outcomes.

Establishing a “medical home” is the first step toward advanced primary care. Broadening the scope and centralizing the role of primary care (and primary care teams), a medical home improves population health, lowers costs, and provides a better, values-based experience for patients.
But where a medical home falls short is in its failure to use data to drive health outcomes across a specific population. And that means a limited ability to address the specific risks of each population.
Like the traditional medical home, the Vera APC model emphasizes the central nature of primary care in a patient’s healthcare journey. Our care teams provide 80-90% of the needed care within the confines of the primary care setting. The difference between a traditional medical home and APC is in the data.
APC leverages a powerful informatics platform to identify the segments of the population that can most benefit from primary care. Usually, these are patients in the at-risk category (20% of the population, 35% of the cost) with at least one underlying condition. By practicing a holistic approach to primary care, our providers can help patients manage those underlying risks while encouraging behavior change that will lead to better health down the line. This segmented approach, combined with smart preventive care for those who fall within the healthy segment of the population, takes the effectiveness of a medical home to a whole new level.
Now, because of our partnership with Castlight Health, we can stretch the capabilities of data even further, using cutting-edge, digital navigation technology that utilizes personalization to spur engagement, encouraging members to take the specific actions that will have the greatest impact on their health. It’s the natural evolution of APC and the concept of a medical home.
At Vera, we analyze over two years of claims data to develop a clearly defined understanding of the risks for each population we serve and the opportunities to improve health outcomes, all the way down to the individual member.
This specificity also helps create the right message to patients, so we can better promote their clinics and communicate why engagement is so important to their health. New digital navigation capabilities also assist in ensuring the information with the greatest potential impact is available to each member.
What are the requirements of every effective APC model? Robust informatics, active care coordination, professional health coaching, and empathetic listening.
Each of the following four capabilities play a crucial role in the model’s ability to deliver improved health outcomes at a lower cost. Let’s take a deeper look:

The APC model leverages an informatics platform that analyzes numerous data sets, including insurance claims and electronic medical record (EMR) data, to ensure optimal care is provided to each population the APC model serves.
Although an informatics platform improves the overall performance of the entire model, there are three essential ways that it contributes to effectively improve the health outcomes for an entire population:

In a typical primary care setting, providers serve as referral machines to specialty care. Instead of having time available to diagnose the cause of a patient’s symptoms, they have to quickly refer the patient out for costly procedures and specialty care that may or may not solve a patient’s actual underlying health issues. In these cases, there’s also little linkage back to the patient's primary care providers.
In the APC model, primary care providers serve as the quarterback of a patient’s care. They and their care teams spend the time in the primary care setting to provide all the care possible. Then, if more care is needed than can be provided at the care center, patients are sent to high-value specialists. Once their specialty care is complete, follow-up is handled in the care center. All of this care is tied together nicely by a care plan.
Active care coordination may seem like a simple concept but it isn’t common. When implemented correctly within the APC model, it has four specific, positive impacts:

In the APC model, clinically integrated behavior change coaches operate as a key part of care teams. Their role is to walk alongside patients using TTM to help patients change their behavior to improve their lifestyle and achieve life goals. These coaches team up with providers and behavioral health professionals to provide whole health care to patients.
Clinically integrated behavior change coaches certified in TTM have a significant impact on the APC model in three specific ways:
The final capability required to effectively implement the APC model is empathetic listening. Empathetic listening builds on active listening, so patients feel truly heard and understood. When physicians, nurses, and health coaches are trained in and employ empathetic listening, they help their patients achieve positive health outcomes.
In many ways, empathetic listening is the core to the success of the APC model. But there are three specific ways that it disproportionately impacts the model’s effectiveness.
You’ve had a chance to learn about the benefits and origin of APC. Are you ready to move forward?
The biggest question payers face when they decide to get into the business of primary care delivery is whether they will build the care delivery system from scratch or buy it by working with an experienced partner.
The right approach will depend on the capabilities of the payer and the speed at which they want to launch a primary care solution to their members.
Your answers to these questions will help you determine the path of least resistance for your efforts to get an APC model up and running. You can learn more about how to think about these questions here.
Self-insured employers face a different challenge than payers. The biggest thing they need to do is flip the paradigm of how they approach benefit strategy design.
Employers are accustomed to the two realities of benefit strategy design within a fee-for-service healthcare system: Costs always go up and, as a result, the benefits they’re able to provide always go down.
Employers are consistently evaluating how to reduce healthcare costs without reducing their workforce’s ability to access needed healthcare. This constant juggle often leads to cost-shifting toward patients in the form of high-deductible health plans. The only problem is, these plans further exacerbate the key problem with the fee-for-service healthcare model — patients who have to pay more for care only go to the doctor when they get really sick.
APC offers a different option, one that encourages patients to seek out care early and often. While it may seem counter-intuitive that increased utilization reduces costs, we’ve proven that this value-based model drives significant savings through reduced claims. In fact, we guarantee this to happen when we work with an employer. You can learn more about how we did this with the City of Kirkland here.
There’s no reason to expect that you must spend 15% more each year on your benefit strategy. You just need to approach the problem differently.
The future of healthcare is being built right now and APC is paving the way. Don’t get left behind. If you’d like to find out more about the APC model and what it can do for you and your organization, let’s talk.