Insights
Resource Library
Keep up with Vera
Join the Vera News community and be the first to learn about interviews with Vera thought leaders & healthcare experts, new resources, and more!
Vera blog

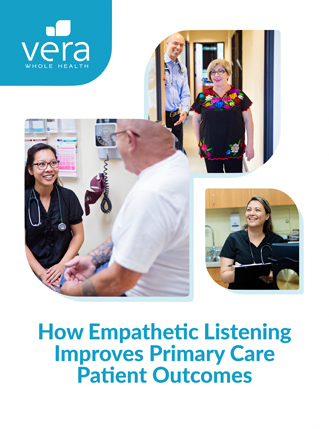
How Vera Employees Are Making A Real Difference
11.23.2022
Advanced primary care (APC) continues to make an impact on health outcomes, engagement, and total cost of care. We’ve long claimed that we’re creating a...